Glass half full? New research highlights link between mindset and outcome of diabetic ulcers
By Simon Jackson, MD at Frontier Medical Group
It’s no secret in the healthcare industry that a patient’s mental state is often directly affected by their physical wellbeing. The two go hand-in-hand and numerous studies over the years have highlighted how a physical illness can impact a person’s general mental state. For example, a strong correlation has been identified between the length of time a patient is in hospital and their level of depression.
Unsurprisingly, it is a reciprocal relationship. Studies have also found that the mindset of patients can have an equally significant influence on their recovery. Mental health however, provides less quantitative data to analyse, and so this is typically a much more difficult correlation to prove.
New research published by the University of Nottingham has tackled the issue, and produced significant results based on a survey of patients suffering from diabetic foot ulcers. Across a five-year period, researchers from the University sought to test the influence of mindset on their treatment and consider the hypothesis that life expectancy in people with diabetic foot ulcers is shorter in patients with negative beliefs regarding their ulcers.
Using a sample size of 169 patients, the researchers recorded their diabetes type, glucose control, number of previous ulcers, infection level and the size and location of their ulcers.
Each patient was given the same advice and treatment for their condition, and completed a survey of their illness beliefs and depression levels. Further data was then collected between four and nine years after their initial interviews, to assess mortality rates and the recovery of patients.
The research found that of the 169 patients, with an average age of 61 and most of whom had type 2 diabetes, 56 had died. It also revealed that on average there were low levels of depression across the group throughout the same period, suggesting there was no obvious link between depression and their condition.
Significantly however, the study did find that patients who believed their ulcers were associated with greater symptoms and feared they would last a long time, died more quickly.
The findings provide evidence that negative beliefs held by a patient about their illness, alongside other clinical factors, may in fact influence survival in people with diabetic foot ulcers. It’s a highly significant conclusion, even it does come from only a small scale case study.
The risk is clear and the cause of the patient’s pessimism is understandable, as while foot ulcers may sound relatively innocuous, people with type 1 and type 2 diabetes are more susceptible owing to nerve damage and the narrowing of the arteries to the feet and lower leg. Any small injuries to the foot can fail to heal and turn into ulcers which can become infected and hard to treat, sometimes leading to amputation and even death.
This study then, could help ensure the healthcare industry is able to better understand mortality risk and how patient attitudes can influence treatment, which ultimately will help shape treatment techniques and save lives.
The challenge however, is for healthcare facilities to provide a solution which aids the treatment and prevention of diabetic foot ulcers, and offers a success rate that patients will have confidence in. As the number of people suffering from diabetes in the UK is rising so rapidly, this has never been more important.
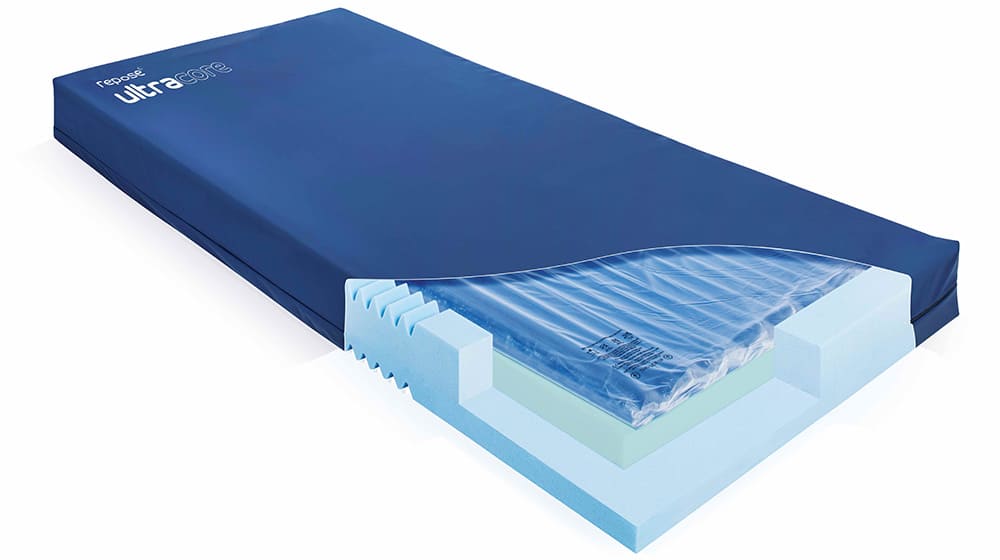
It’s a challenge that we’ve seen evolve and an area where Frontier Medical Group has significant experience, as our Repose range is specifically designed for the prevention and treatment of pressure ulcers, including diabetic foot ulcers. We’ve spent more than 18 years researching and developing our range of products which offer a comfortable solution for patients suffering from foot ulcers, or in fact any form of pressure damage.
We have seen first-hand how effective the treatment offered by the Repose range is, not only in terms of physical care but in the benefits to a patient’s mental state that come as a consequence, and that’s something which should appeal to both patients and healthcare professionals. It’s one of the reasons why we have been able to develop a long standing partnership to supply the NHS, and why more than three million patients now use Repose products throughout Europe.
It also allows us to continually innovate and expand our range to meet demand, as represented by the introduction of Ultracore, a new hybrid mattress designed to aid the prevention and treatment of pressure ulcers, earlier this year.
Ultimately, we believe our approach as a company links closely to the research and findings from Nottingham University. Hospitals and healthcare professionals are responsible for the treatment and the recovery of their patients and while the most obvious part of that concerns their physical health, they have an underlying duty of care to support them mentally as well, to the best of their ability.
Whether that means providing the appropriate products to support them, or offering a level of therapeutic treatment to support their care, the resources are available out there and we should ensure they are used to the best of our advantage. Where possible, the patient’s glass should always be half full, rather than half empty, as in the long run it’s going to have a better outcome for everyone.
Simon Jackson is MD at market leading Frontier Medical Group. For more information, visit www.frontier-group.co.uk